Could You Have A High Level Of Cortisol? What Every Patient Needs To Know
Do you have diabetes that is difficult to control despite being on multiple medications? An abnormally high level of cortisol in your body could be a factor.¹
Excessively high levels of cortisol in your body could be due to a condition known as hypercortisolism or Cushing syndrome. Some classic symptoms of Cushing syndrome include a round and reddened face (moon face), fatty hump between the shoulders (buffalo hump), & purple stretch marks on the abdomen (striae).¹
However, there are more subtle presentations of Cushing syndrome as well. Most people will not have the classic symptoms of Cushing syndrome, but rather a combination of other medical conditions.¹
Let’s learn more about this by first understanding cortisol.
What Is Cortisol?
Cortisol is a hormone produced by the adrenal glands. The adrenal glands sit on top of the kidneys, and there is one adrenal gland on each side of the body. Cortisol is necessary for your body to function normally. When your body undergoes stress (emotional or physical) the natural response is for your body to produce excess cortisol. Examples of physical stress include hospitalization, having surgery, or being in pain.¹ Emotional and psychological stress, such as depression, can also lead to excess cortisol production by your body.¹
Although cortisol is a stress hormone, day to day stress will not cause your body to produce excessive levels of cortisol for a prolonged period of time.
Types Of Cushing Syndrome
Cushing syndrome is the result of a prolonged elevated level of cortisol. This is usually from a specific source. This source may be a tumor which could be from one or both of the adrenal glands or of pituitary origin. Other causes of Cushing syndrome include an ectopic source of cortisol (such as a tumor somewhere else in the body), or iatrogenic (patients taking steroid medications).¹
The type of Cushing syndrome depends on the source of the excess cortisol. Let’s take a deeper look at nodules causing Cushing syndrome. As mentioned above this could be a pituitary nodule or an adrenal nodule.
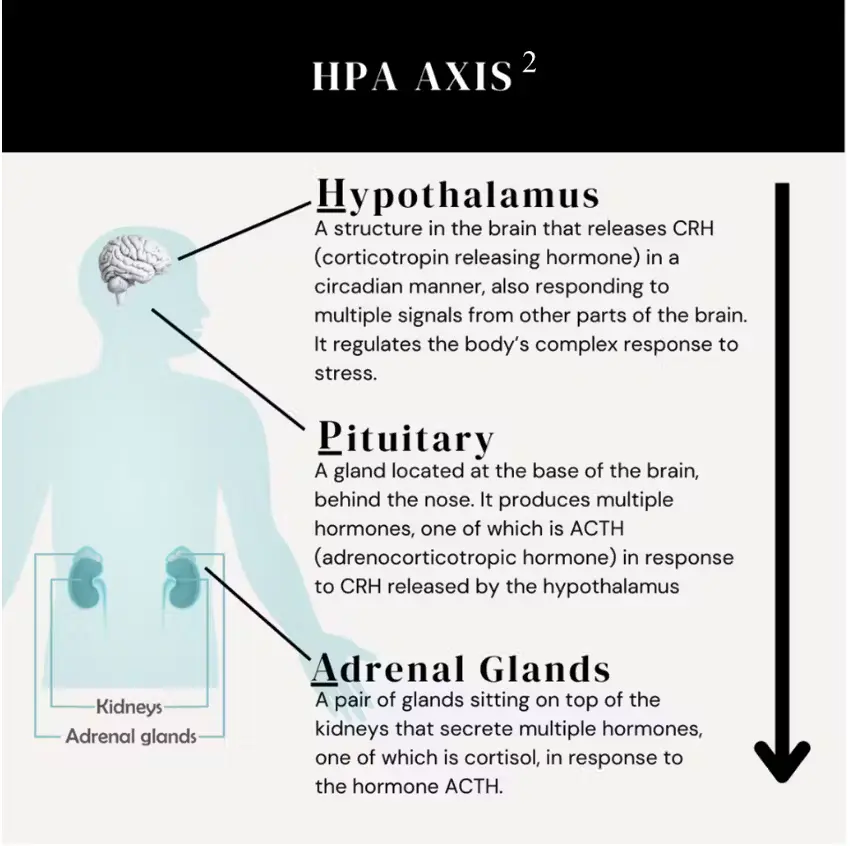
An adrenal nodule or adrenal incidentaloma will produce excess cortisol itself.¹ This is in contrast to a pituitary nodule which will increase cortisol by increasing ACTH production through the body’s HPA axis.¹
The hypothalamus secretes corticotropin releasing hormone (CRH) which then signals the pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH travels to the adrenal glands to stimulate the secretion of cortisol.²
A pituitary gland tumor is typically found through imaging of the pituitary gland or the thoracic area.¹
An adrenal gland tumor is discovered in one of two ways.
- Signs and Symptoms Of High Cortisol – A patient presents with high cortisol signs and symptoms. To confirm a doctor’s suspicion of excess cortisol, blood or urine tests are usually ordered. If the tests performed are positive, an imaging study may be done to search for an adrenal gland tumor.¹
- Adrenal Nodule Found Incidentally – A patient has an imaging study done of their abdomen for a cause unrelated to high cortisol. An adrenal nodule is found incidentally by the radiologist or the ordering physician.³
All adrenal adenomas should be worked up by a doctor.¹ This testing will help to determine if the adrenal adenoma is producing an excess level of hormone. Because the adrenal gland produces many different hormones, the excess hormone made by the adenoma could be cortisol, aldosterone, DHEA sulfate, catecholamines, or metanephrines. In the case of Cushing syndrome caused by an adrenal adenoma, the excess hormone produced is cortisol.⁴
Signs and Symptoms Of Cushing Syndrome
A person may present to their doctor with classic physical features of Cushing syndrome. This may include moon face, buffalo hump and abdominal striae. Some may not have the classic appearance, but rather could have Type 2 diabetes, hypertension, osteoporosis, or polycystic ovarian syndrome, which are also common conditions of Cushing syndrome. Other symptoms experienced by patients may include fatigue, sleep disturbances, and weight gain. The weight gain from a high cortisol level can be seen more often in the face and the abdomen.¹
As with any medical condition, the degree of severity in the signs and symptoms of Cushing syndrome can vary. A person may or may not have obvious physical features of Cushing syndrome. Rather, the patient may have a medical condition like the ones mentioned above. Because each person has different signs and symptoms, diagnosing Cushing syndrome can be challenging.¹
Diagnosing Cushing Syndrome
If Cushing syndrome is suspected, a doctor will need to determine the source of cortisol excess. The sources of cortisol excess may come from a pituitary nodule, an adrenal nodule, or a tumor elsewhere in the body.²
Cushing Syndrome Is A Spectrum
The level of hypercortisolism may play a role in how clinically obvious Cushing syndrome is in a person. In subtle presentations of hypercortisolism, a patient may only have weight gain, fatigue, a chronic disease like diabetes or Polycystic Ovary Syndrome (PCOS), or decreased concentration. In women, a high level of continuous cortisol oversecretion can also lead to excess facial and body hair (hirsutism), female balding, and irregular menstrual periods.¹
Although patients with a mild presentation may not have the overt features of moon facies or easy bruising, they can still be negatively impacted by hypercortisolism in different ways, such as difficult to control diabetes. In one study, 2% to 3.5% of patients who were referred for poorly controlled diabetes mellitus had confirmed hypercortisolism after a work up. Some of these patients had adrenal adenomas that were not diagnosed until being referred for a workup for Cushing syndrome.⁶
In a more overt Cushing syndrome presentation, a patient may have reddish purple abdominal striae, skin that is easily bruised, and unexplained osteoporosis.¹ Their face may be more rounded and bloated (called facial plethora or moon facies). Similar to mild presentations, severe cases of Cushing syndrome are also likely to have high blood pressure, poorly controlled diabetes, weight gain, and the features present in mild cases.¹
Treating Cushing Syndrome
Surgery is typically the first option for treating Cushing syndrome. For patients who cannot have surgery, radiotherapy and / or medical therapy are also options. There are multiple medications that may help treat the symptoms of hypercortisolism.⁵
Elevated Cortisol: Take Home Points
Cortisol is an adrenal hormone that is secreted normally as a response to both physical and emotional stress. Cushing syndrome or hypercortisolism happens when you have a sustained and higher than normal level of cortisol in the body.¹
Severely high levels of cortisol may cause classic physical features of Cushing syndrome. Mildly elevated levels of cortisol may not be as obvious. Nevertheless, even mildly elevated levels of cortisol can lead to metabolic effects that affect your long term health and quality of life.⁷ To diagnose Cushing syndrome, typically both laboratory tests are done and imaging studies. It is a complex condition that if left untreated can cause worsening medical conditions.¹
Adrenal nodules may be picked up incidentally on imaging studies that were ordered for other reasons. If an adrenal nodule is found on an imaging study, it should always be worked up for high cortisol.¹
Sources:
- Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93(5):1526-1540.
https://pubmed.ncbi.nlm.nih.gov/18334580/ - Raff H, Carroll T. Cushing’s syndrome: from physiological principles to diagnosis and clinical care. J Physiol. 2015;593(3):493-506.
https://pubmed.ncbi.nlm.nih.gov/25480800/ - Bancos I, Taylor AE, Chortis V, et al. Urine steroid metabolomics for the differential diagnosis of adrenal incidentalomas in the EURINE-ACT study: a prospective test validation study. Lancet Diabetes Endocrinol. 2020;8(9):773-781.
https://pubmed.ncbi.nlm.nih.gov/32711725/ - Sherlock M, Scarsbrook A, Abbas A, et al. Adrenal Incidentaloma. Endocr Rev. 2020;41(6):775-820.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7431180/ - Newell-Price J, Bertagna X, Grossman AB, Nieman LK. Cushing’s syndrome. Lancet. 2006;367(9522):1605-1617.
https://pubmed.ncbi.nlm.nih.gov/16698415/ - Catargi B, Rigalleau V, Poussin A, et al. Occult Cushing’s syndrome in type-2 diabetes. J Clin Endocrinol Metab. 2003;88(12):5808-5813.
https://pubmed.ncbi.nlm.nih.gov/14671173/ - Di Dalmazi G, Vicennati V, Garelli S, et al. Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol. 2014;2(5):396-405. doi:10.1016/S2213-8587(13)70211-0
https://pubmed.ncbi.nlm.nih.gov/24795253/
This is sponsored by Corcept Therapeutics. For more information on cortisol please visit CortisolMatters.com. DSE-00995 NOV 2022
We discuss products we think are useful to people. If you buy something through our links, we may earn a commission. Remember to check with your personal physician to see if a product recommended is right for you.